by Lara Kassel | Jan 16, 2024 | Policy & Budget Agenda
Download our agenda here.
Find our testimony to the Assembly Ways and Means and Senate Finance Committees on the 2024-2025 Executive budget here.
Our one-pager highlighting our positions on the Governor’s proposed 2024-2025 budget is here.
Find a summary of the Governor’s adult mental health proposals for 2024 by the Urban Justice Center Mental Health Project here.
New York State will soon embark on extensive health equity reform through the approval of an amendment to the Medicaid 1115 Waiver. The initiatives proposed in the amendment are worthy, though are not enough to eliminate systemic inequities. Medicaid Matters has long brought recommendations to the table to do that, which would go a long way to eliminating inequities across our systems of care and services to people with low income and people with disabilities who are served by Medicaid and other public programs.
Expand access to public health insurance programs and services
New Yorkers should have access to comprehensive insurance coverage, regardless of their circumstances. Universal health coverage, which Medicaid Matters supports, would guarantee this as a right. In the meantime, we must work toward making improvements to public programs and access.
New York must advance health equity by providing needed coverage for older adults, people with disabilities, immigrants, and children by:
- Creating a state-funded Essential Plan for all low-income New Yorkers, regardless of immigration status to provide coverage to immigrants not eligible for insurance due to their immigration status.
- Providing continuous coverage in Medicaid and Child Health Plus from birth to age six;
- Aligning the asset limit for people with disabilities and older adults with the new asset limit enacted in the expansion of the Medicaid Buy-In Program for Working People with Disabilities in 2023; eliminating the asset test thereafter.
Strengthen Medicaid managed care
New York has administered Medicaid through managed care plans since the mid-1990s. In 2011, the Department of Health was authorized to expand managed care to people and benefits previously excluded or exempt from mandatory managed care participation. Over the years, appropriate and effective State oversight of the operation of managed care plans has diminished. This has resulted in less access to needed care and services.
To protect New Yorkers enrolled in Medicaid managed care, the State must:
- Strengthen and enforce continuity of care and transition rights, particularly in Managed Long Term Care;
- Address capacity concerns to ensure that Medicaid enrollees have timely access to medical, mental health and dental providers;
- Enhance transparency by posting Managed Medicaid Cost and Operating Reports (MMCOR) data and other data sets that demonstrate plan activity, like denials;
- Address systemic inequities by collecting and reporting managed care data based on race, ethnicity and disability, at a minimum;
- Add health equity standards to the model contracts and managed care rate setting methodologies;
- Revamp the Department of Health system for taking and addressing complaints and use individual complaints to identify systemic issues.
Abandon potential move to managed care for people with I/DD or other waiver populations
Medicaid Matters urges the State to abandon ideas to move the system of services for people with intellectual/developmental disabilities (I/DD) or people who are served through other Medicaid waiver services, such as the Nursing Home Transition and Diversion waiver, to Medicaid managed care. New York has been exploring the possibility of managed care for people with I/DD for over ten years, however, studies from other states have shown there are no savings associated with managed care for this group of people, and there is no evidence of improvements to access or quality of services.
Ensure access to home and community-based services
People have a right to live independently in their own homes in the community. Despite these rights, people suffer without home care and risk facility placement due to high turnover and workforce shortages. New York must strengthen the workforce that supports them and remove barriers to accessing services by:
- Enacting Fair Pay for Home Care;
- Investing in higher wages for direct support professionals who support people with I/DD;
- Implementing a robust, independent advocacy assistance program for people with I/DD; and
- Repealing restrictions to the Managed Long Term Care program enacted in 2020 (requirements based on needing assistance with at least three activities of daily living, and the addition of the look-back period for income eligibility for community-based long-term care).
While some improvements to community-based services have been made, the State must invest more heavily in community-based mental health care to ensure higher quality and greater access to needed services (as the State did with significant investments in hospital-based mental health care in recent years). New investments should be made to enhance quality in congregate residences operated by the Office of Mental Health, clinics, and psychiatric units, as well as to promote access to community supports and services for people with serious mental illness.
Maintain unimpeded access to pharmacy benefits.
In 2023, most Medicaid enrollees had their pharmacy benefits moved from Medicaid managed care to NYRx, the pharmacy benefit program managed directly by the State, with the goal of improving access to medications. Since the transition, some people have encountered problems receiving their medications, are not receiving any written notice, and are uncertain of what to do if their medically necessary prescription cannot be filled. While we recognize NYRx has been working to address these problems on a case-by-case basis, this should only be a stop-gap measure. We urge NYRx to develop a systemic approach for helping people who experience problems with prescriptions, including providing timely and clearly written notices of denials, so people covered by Medicaid have unimpeded access to the medications they need.
Restore transparency to the Medicaid budget New York’s Medicaid spending cap was presented in 2011 as a mechanism to limit growth in Medicaid spending and instill discipline in Medicaid budgeting. It has allowed the administration to justify Medicaid cuts and drastic changes that diminish access to services. Medicaid Matters believes the cap should be replaced with intelligent budgeting which would allow the State to make necessary investments and adjustments reflective of real-world needs and conditions. If the cap is kept in place, the State should be required to report monthly on Medicaid spending rather than quarterly. In addition, the Division of the Budget should publish plain language summaries to accompany their cap reports and should provide public webinars with live Q&A or other similar opportunities for transparent information sharing about the Medicaid budget.

by Lara Kassel | Jan 10, 2024 | News
Download a PDF of this statement here.
New York has long been a leader in providing affordable, comprehensive coverage in public health insurance programs. Governor Hochul has built on this legacy by raising Medicaid income eligibility for older adults and people with disabilities, expanding the Medicaid Buy-In for Working People with Disabilities, and more. Now New York is poised to become the next state to provide continuous coverage in Medicaid and Child Health Plus for the youngest New Yorkers through an intent to apply for Section 1115 Medicaid Waiver authority to do so.
Enacting continuous coverage for children until they reach age six will keep New York on the forefront of protecting and investing in our youngest children and their families across the state.
“New York has been a national leader when it comes to improving and expanding healthcare coverage. Now our state will continue this legacy by protecting children from having gaps in coverage, which can have profound consequences on their health, education, and the financial security of their families” said Elisabeth R. Benjamin, Vice President of Health Initiatives at the Community Service Society. “Providing continuous coverage to children under the age of six is the right thing to do from a policy and fiscal perspective. CSS commends Governor Hochul for making this commitment.”
“This is exactly the right focus for ensuring the health of New Yorkers. Investing early in children promotes health for a lifetime and is the most important thing we can do for future health and healthcare savings,” said Jeff Kaczorowski, MD, NYS American Academy of Pediatrics.
“New York has long been a leader in providing public health insurance coverage, like Medicaid and Child Health Plus, to people with low income across our state. These programs are the reason millions of New Yorkers can access needed care and services, especially children. Parents and caregivers have enough on their plates without having to worry about enrollment paperwork. Several other states have eliminated annual paperwork barriers by providing continuous coverage, and I’m so proud New York is ready to be next.” said Lara Kassel, Coalition Coordinator, Medicaid Matters New York.
“I am a parent of a child on the Autism Spectrum. He was diagnosed at two-and-a-half years old, and Medicaid served as a lifeline for us from the start for key services and supports. Throughout his life, he’s had gaps in medical care as a consequence of the re-enrollment process. As a former family in temporary housing transitioning out of that system, and with the change of address and circumstances, the enrollment process was very complicated for us, leaving my son and I uninsured for some time. Providing continuous coverage for young children will ensure these strenuous processes don’t result in families becoming uninsured even when they do qualify for Medicaid,” said Maggie Sanchez, parent in Queens, New York.
“Robin Hood applauds Governor Hochul’s announcement today that she will seek a federal waiver to provide continuous Medicaid coverage to children 0-6 years of age. At least two states have now adopted a multi-year continuous coverage model for young children, while several others are considering similar reforms. New York has an opportunity to better protect low-income young children and their caregivers by eliminating gaps in coverage caused by needless procedural burdens. Poverty is a policy choice and we have an opportunity here to make the right choice for our children,” said Richard R. Buery, Jr., CEO of Robin Hood, New York City’s largest local poverty fighting philanthropy. “This announcement by the Governor follows the critical leadership of Assemblymember Jessica González-Rojas and State Senator Samra Brouk on this issue through their co-sponsorship of A8146/S7747, which would codify into law continuous Medicaidcoverage to eligible children from when they are first enrolled in Medicaid until the age of six.”
“Keeping New York’s children and babies insured means keeping them healthy. Continuous health care coverage from ages 0-6 means parents can access regular check-ups, scheduled vaccines, and preventive health services for their child during the crucial early years, giving them a healthy start. Even a short gap in health insurance coverage can result in a child missing needed care and interventions. The Schuyler Center thanks Governor Hochul for including this important proposal in her State of the State address. A budget that supports the health and well-being of all of New York’s children is crucial to the future of our state,” said Kate Breslin, President and CEO, Schuyler Center for Analysis and Advocacy.
“Children shouldn’t lose access to healthcare simply because their parents picked up some seasonal work or a bit of overtime,” said Larry Marx, CEO of The Children’s Agenda. “But that’s what happens when parents temporarily earn too much for their children to qualify for Medicaid. We have to stop the revolving door of healthcare access. Continuous Medicaid coverage from birth to 6 years is a commonsense solution that’s good for kids. Ensuring continuity of care in the early years will save money in the long run and it’s the right thing to do. Healthy kids succeed in school and in life.”
“Continuous coverage from birth to age 6 years is a game changer for New York’s children and families. By eliminating disruptions in health insurance coverage, New York State creates a foundation for equitable access to preventive healthcare and care for illness and injuries throughout early childhood to keep our babies healthy,” said Laura Jean Shipley, MD, UR Medicine/Golisano Children’s Hospital.
“We see the cumulative effect of the circumstances that qualify our adult clients for Medicaid in the first place, and it’s why any disruption in Medicaid coverage for children has an exacerbated impact on low-income families,” said Rachel Holtzman, Equal Justice Works Fellow with the New York Legal Assistance Group. “These are families already navigating economic hardship in an inequitable healthcare system. They’re already facing significant obstacles in accessing the critical care their children need at home and in their communities—obstacles Medicaid is meant to alleviate—and disruptions to the very coverage designed to ensure that access, shouldn’t be one of them.”
This waiver will ensure substantial matching federal funds for a low-cost policy option that will reap many benefits for our state, including:
- Greater health equity. Continuous coverage protections advance health equity by ensuring continuity of treatment for low-income children and children of color, who disproportionately experience health disparities.
- Better child and family health. Continuity of coverage supports proven pediatric interventions, including developmental screening, prevention, and family-oriented two-generation services.
- Reduced costs for families and lower administrative costs. Cycling on and off Medicaid/CHP burdens families with out-of-pocket expenses and stressful deadlines; it also results in higher administrative costs for the state, insurers, and providers.
Stabilized preventive and pediatric health care systems. Gaps in children’s coverage strain the finances of the primary care and pediatric infrastructure of our state. These providers already work long hours for lower reimbursement rates. Ensuring that their patients have continuous coverage will mean this vital component of our healthcare system will flourish.

by Lara Kassel | Dec 11, 2023 | News
Medicaid Matters New York and partner organizations have sent two letters to Governor Hochul urging her to include two eligibility expansions in her Executive budget.
One letter urges the Governor to include authority to provide continuous eligibility in Medicaid and Child Health Plus from birth (or whenever a child enrolls) to age six. Find that letter here.
The other letter urges the Governor to include an increase in the Medicaid asset limit for older people and people with disabilities, followed by repeal of the asset test altogether, in the Executive budget. Find that letter here.
by Lara Kassel | Dec 4, 2023 | News
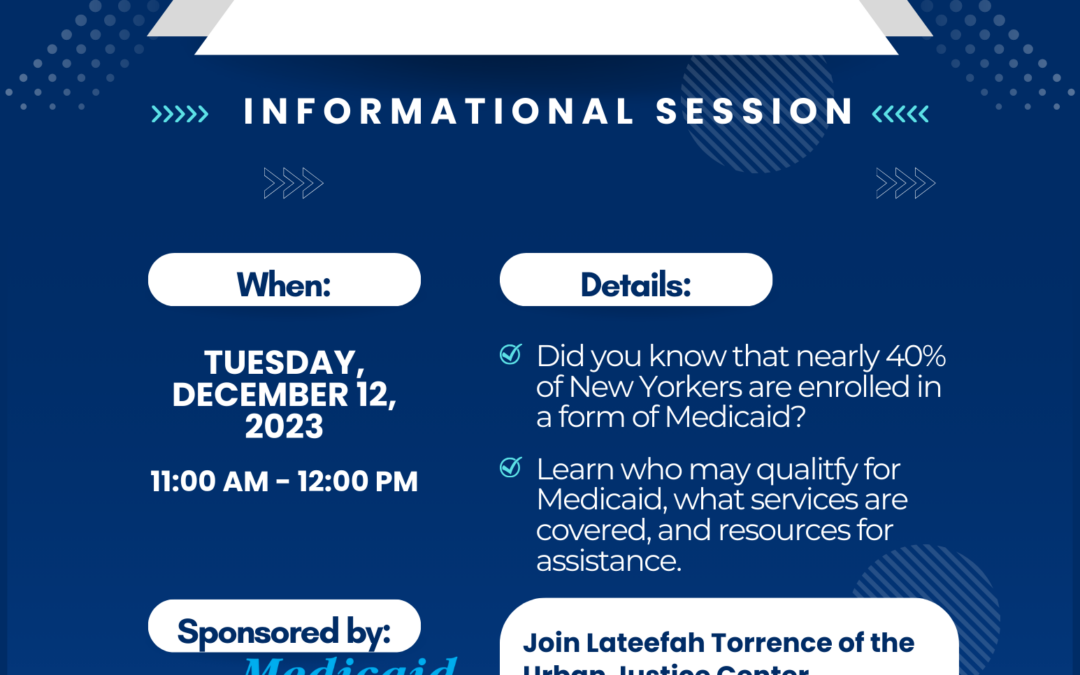
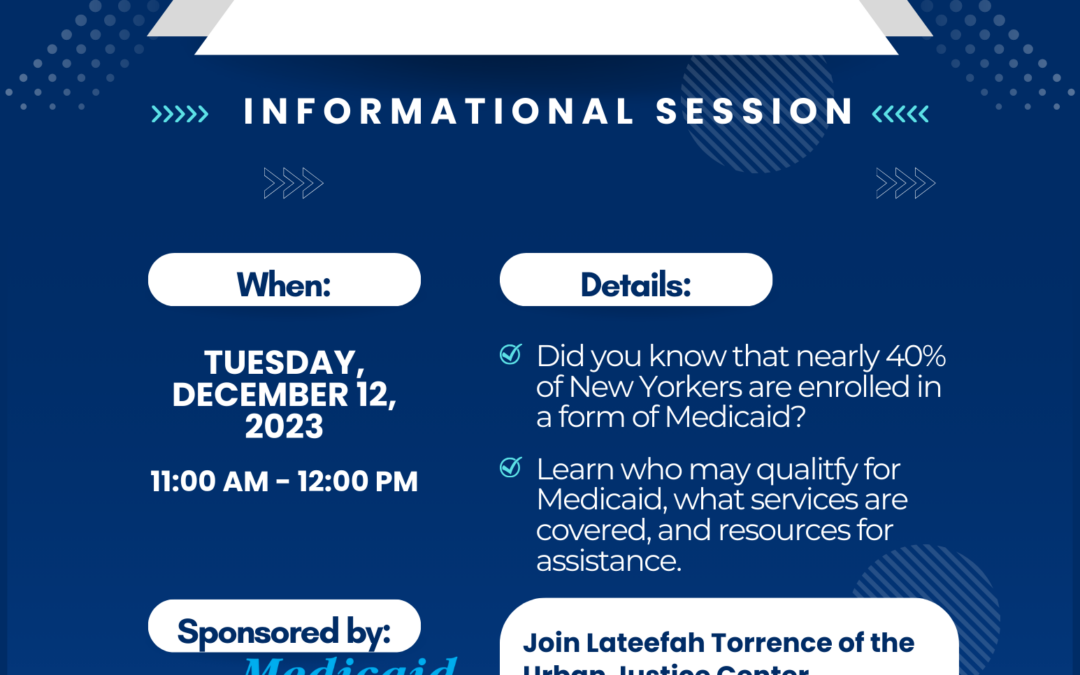
Join an informational webinar, “Medicaid 101,” on Tuesday, December 12, 2023, 11am-12pm. Registration is open here.
Lateefah Torrence of the Urban Justice Center Mental Health Project will provide a plain-language overview of New York’s Medicaid program. Information will include who may qualify, what services are covered, and more.
The webinar will be recorded and will be available to review after the live presentation.
All are welcome!
The webinar recording can be found here and the webinar slides can be found here.

by Lara Kassel | Oct 23, 2023 | Managed Care, News
The NYS Department of Health has announced an expansion of the NY Independent Assessor Program (NYIAP) to include reassessments beginning January 1, 2024. The planned expansion is too soon and the timeline for rolling it out is too aggressive to provide enough assurance people will not lose access to services they need.
Advocates have raised concerns and made suggestions for consumer protections since the NYIAP was implemented, including in a letter to the Department of Health alongside the Coalition to Protect the Rights of New York’s Dual-Eligibles and managed care plan representatives in October 2022 (linked here).
The October 2023 letter urging delay and slow roll-out of the expansion can be downloaded here.




Recent Comments